Musculoskeletal Injury Prevention COMMUNITY
Workplace injuries can be prevented — whether you work in a lab, move boxes, or spend hours working at a computer. This module is intended to help you reduce your risk of suffering Musculoskeletal injury (MSIs).
CASE STUDY
What are the greatest MSI risks for Jane and Maria?

Case Study 1
Jane is a community occupational therapist who spends much of her day assessing and treating clients in their homes.

Case Study 2
Maria is a community health nurse who spends her day providing nursing care to clients in their homes.
3 KEY THINGS
The most important information I need to know.
Signs & Symptoms
3 Stages of MSI
5 Risk Factors
Overview
MSIs are injuries that affect the human body’s movement or musculoskeletal system (i.e. muscles, tendons, ligaments, nerves, discs, blood vessels, etc.). MSI can worsen over time. Early recognition is critical for timely intervention and treatment. It’s also important to recognize the signs and symptoms so they can be reported to your supervisor.

Signs
Signs are things you can see such as:
- redness
- swelling

Symptoms
Symptoms are things you can feel such as:
- numbness
- tingling
- spasms
- stiffness
- reduced range of motion
| 1 |
Early Stage
|
| 2 |
Middle Stage
|
| 3 |
Late Stage
|
WHAT CAN I DO?
Tips to help me take care and stay safe.
Identify workplace risk factors
The first step to reducing MSI is to recognize risk factors and report them to your supervisor.
Problem solve
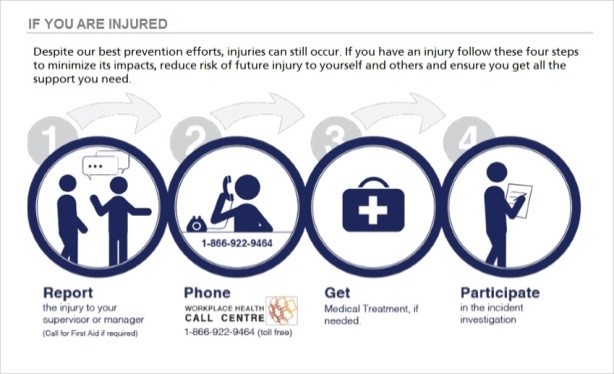
Discuss ways to minimize identified risk factors with your supervisor and peers. If you feel the onset of MSI, consult with your health care practitioner. Early intervention is key to recovery. Report to Workplace Health Call Centre: 1 (866) 922-9464.
Point of care risk assessment
S – Self
- Do I have the skills?
- Am I in the right frame of mind?
T – Task
- Do I know how the patient does the task?
- Has the care plan changed? Kardex? Report?
E – Environment
- Is the area safe?
- Proper equipment and set-up?
P – Patient/Resident/Client
- Is the patient safe to do the planned task?
- Has the patient changed?
- Is this the right time for the patient?
- If transferring: “S.A.F.E. Pre-transfer Check”
Pre-transfer check
Use it to assess if a manual transfer is safe to do at a point in time. There are 5 steps.
- Step 1: Can the patient follow simple instructions and cooperate?
- Step 2: When in bed, can they lift their hips up (bridge) or shift hips (scoot) to the side?
- Step 3: In sitting, can they sit upright independently, and lean forward and back?
- Step 4: Can they start to stand by leaning forward and lifting their bottom off the seat?
- Step 5: In standing, can they move their feet (step on the spot or shuffle their feet side to side)?
The patient must be able to complete all steps to continue with a manual transfer safely.
If the task is unsafe:
- Follow your worksite’s standard procedure for when unsafe work conditions are identified
- Make sure the patient is safe and ask for supervisor input on an alternative plan
- Understand your Right to Refuse Unsafe Work (Occupational Health and Safety Regulation). Refer to Refusal of Unsafe Work Process — the Occupational Health and Safety Agency for health care in BC.
- Familiarize yourself with examples of immediate actions and follow up actions
Correct body mechanics
Correct body mechanics help you position and move your body in a safe and efficient way. They may help reduce muscle fatigue and injury risk.
Apply them in all situations – whether doing patient handling tasks (such as transfers, toileting, bathing) manually or using patient lifts, and when handling materials or other equipment.
Follow these principles of correct body mechanics:
Before you move / lift:
- Assess the work or load
- Get close to the object/person before you move
- Place your feet shoulder width apart in standing or wider if shifting your weight
- Keep your back neutral/straight – Avoid awkward postures
- Do not twist or overreach
During the move / lift:
- Pull your stomach in
- Lift with large leg muscles
- Weight shift using your legs to move
- Lift or move in a controlled way
Know your equipment and tasks
Ask about any Safe Work Procedures (SWP) in your unit/work-area. There are often several different ways to do the same task or activity, and some of these will be safer than others. Review helpful resources on safe use of equipment.
PRACTICE
Checking my confidence in this subject.
MY ACTION ITEMS
Identify risk factors in your new work environment and prepare to discuss problem solving methods when you meet your supervisor and peers in person.
Click here to access & complete the required MSIP quiz.